By Dr. Anna Reid
Writer, curator and historian of art
Art Hx 2021-2022 Interpretive Fellow
Art Hx researchers have located a range of images that speak to the strategic development and significance of medicines in British colonial and postcolonial contexts. Inspired by their work, I have gathered four images that are notable in their promotional or press aspect, their diverse, specific geographies, and in the questions that they raise about the uneven structures of medical research.
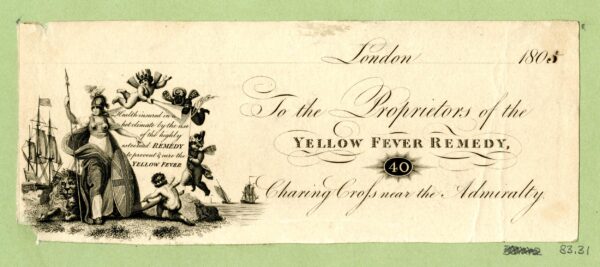
Draft Bill-head of a pharmacist selling a remedy for Yellow Fever, 1805. © Trustees of the British Museum. NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
The 1805 billhead of a company selling a “remedy and cure” for yellow fever offers a way into this constellation as an exploration of four charged images. It will glimpse and point to a long and present history of the public representation of British colonial medical treatments, images which the constellation contextualizes in their links to the extractive logic of empire. The billhead, printed and distributed as a paper receipt to purchasers of the purported remedy, features the figure of Britannia, a personification of Britain. The deified female warrior, armored and shielded, is served by cherubic figures, some with darker skin tones, indicative of colonized lands and subjects. The strength, health, and fecundity of the protagonist becomes the promise of this medicine, as a prophylactic against the scourge of tropical disease. Yellow fever, so called because of the disease’s symptom of jaundice owing to liver damage, was transmitted from its origins in Africa to the Americas as a result of the trafficking of enslaved people across the Atlantic Ocean since the sixteenth century. Accessible via the admiralty, this costly commodity was devised for the use of imperial administrators.
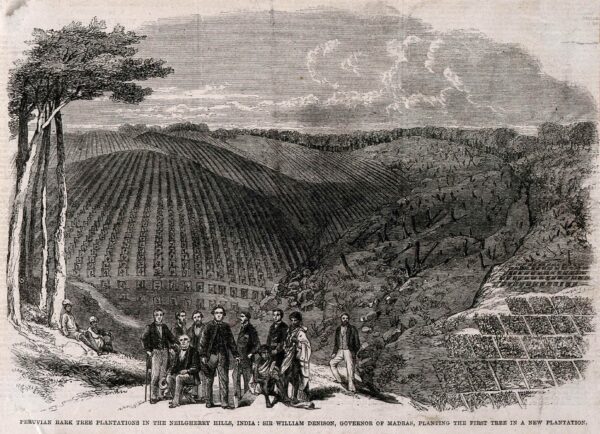
Sir W. Denison and others planting the first quinine tree in the Neilgherry hills, India. Wood engraving by M. Jackson, 1862. Credit: Wellcome Collection. Attribution 4.0 International (CC BY 4.0)
Another print, dated to 1862 and also making representations on behalf of empire, extends this consideration of the development, production, and use of tropical medicine. Shared as an illustration for The London Magazine, the print is a picturesque depiction of the Neilgherry Hills, as a colonized territory of India (a district of the Madras Presidency, covering southern India and then-named Ceylon). William Dension, the main protagonist of the image, became governor of Madras in 1861. The rolling contours depicted beneath a buoyant sky imply an open, temperate landscape, which on closer inspection is a vast clearing prepared for the planting of cinchona trees, the source of the antimalarial quinine, native to western South America. With the ceremonial placing of the first tree marked in this engraving, cultivation begins, and immense yields are implied: the poised colonial administrators claim and oversee the land, worked by colonized subjects here represented in three figures posed to indicate balance and cooperation. As stocks of “the Peruvian bark” were depleted by the mid-nineteenth century, this experimental new cultivation in India was of key strategic importance to the occupation and administration of the tropical colonies. The historical and cultural role and significance of Indigenous medicinal plants was lost when the cultivation of cinchona was introduced in colonial India.[1] A diverse range of Indigenous peoples—Todas, Kotas, Badagas, Irulas, and Kurumbas—continue to inhabit the Neilgherry Hills. The role of the traditional ecological knowledge of the Todos has been emphasized in the contemporary work of repairing the area’s significant indigenous biodiversity, which was dramatically afflicted by the British company and crown governments in the nineteenth century.[2]
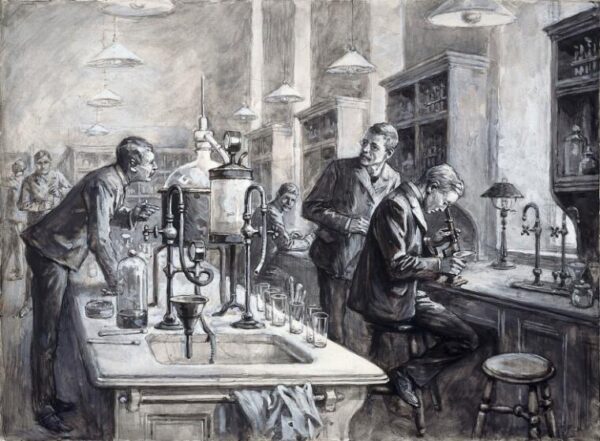
Sir Ronald Ross, C.S. Sherrington, and R.W. Boyce in a laboratory at the Liverpool School of Tropical Medicine. Gouache by W.T. Maud, 1899. Credit: Wellcome Collection. Public Domain Mark
Made by a press artist, a gouache (a type of painting created using an opaque watercolor technique) of researchers at the Liverpool School of Tropical Medicine at the time of its inauguration similarly projects an image of resilience and medical preparedness. It documents the formalization of the Tropical Medicine field in the establishment of the first school dedicated to its study in 1898 and the use of the microscope in line with the evolving germ theory of disease. As a major seat of empire, the port city of Liverpool was frequently afflicted by “tropical” disease. Outstanding physicians and scientists took up prestigious positions at the new institution, notably Ronald Ross who in 1897 discovered the malarial parasite in the gastrointestinal tract of a mosquito, thus generating new understanding of the disease’s transmission. In tracing a long development of the concept of tropical medicine through imperial history as investment in the healthcare of European troops and settler populations in the tropics, historian of medicine and empire Pratik Chakrabarti notes the Liverpool School’s work training doctors for colonial service in “a medicine for empire where diseases were the great enemies of civilisation.” Nineteenth-century Africa, he remarks, was seen as a “white man’s grave.”[3] The Liverpool School was founded by and with the financial support of Alfred Lewis Jones, a shipping magnate with expansive interests in Jamaica and West Africa and a close engagement with the “Belgian Congo” and King Leopold II, who also made substantial donations to the school.

Scientists working at the LSHTM malaria lab. Image courtesy the London School of Hygiene & Tropical Medicine
A contemporary press photograph offers a way to complete this constellation, returning us to questions about the colonial nature of extraction, medical treatments, their efficacy, and their circulation. The image foregrounds a researcher at work in a state of the art laboratory, and it was used to announce research which has identified genetic variants in malaria parasites that enable them to infect individuals previously thought to have strong protection against the disease. The research is produced by the London School of Hygiene and Tropical Medicine with major partners and its own Medical Research Council (MRC) Unit The Gambia. Since 1947, MRC The Gambia has led “health research in West Africa to save lives and improve health across the world” and serves as the hub of its West Africa Research Programme.[4] Funders include a range of non-governmental organizations and pharmaceutical companies. It is also supported by the predominant global health organization, the WHO.[5] “Global Health” is a term that now supersedes Tropical Medicine as a discipline inseparable from the history of colonialism. In 2021, LSHTM researcher Lioba A. Hirsch has asked, is it possible to decolonize global health institutions? She proceeds:
If we want to work towards health justice, the institutions that have been built on and benefitted from the racist exploitation of Black, Brown and Indigenous populations the world over cannot decolonize and keep their epistemic, political and financial power… Anti-racism and decolonization do not simply mean being nicer to staff of colour and people from LMICs [low and middle income countries]. It means cutting those people off who have benefitted from the system and used their privilege to discriminate against others or let an oppressive system go unchallenged… If we have learnt one thing from historical processes of decolonisation, it is that global missions should fill all of us with dread, even if they are designed to do good and improve local conditions. That is how colonialism was justified and how global health sees itself.[6]
As a field of research, contemporary global health evolved from an imperial history throughout which the development of medicines to protect colonists and their interests was of paramount strategic priority. The images discussed here variously project and circulate colonial and postcolonial advancements in the understanding and management of disease, and as a constellation, they invite and aid critical considerations of what an image of decolonized medical research might look like.
[1] Abhijit Mukherjee, “The Peruvian Bark Revisited: A Critique of British Cinchona Policy in Colonial India,” Bengal, past & present : journal of the Calcutta Historical Society Vol. 117 (1998): 81-102.
[2] Rodrigo León Cordero et al., “Elements of indigenous socio-ecological knowledge show resilience despite ecosystem changes in the forest-grasslands mosaics of the Nilgiri Hills, India,” Palgrave Communications Vol. 4, (2018): 1-9.
[3] Pratik Chakrabarti, Medicine and Empire 1600-1960 (Basingstoke: Palgrave Macmillan, 2013), 141-163.
[4] “MRC Gambia,” London School of Hygiene & Tropical Medicine, accessed January 31, 2022, https://www.lshtm.ac.uk/research/units/mrc-gambia.
[5] In the context of a global pandemic, it is noteworthy that as of February 15, 2022, just 349,875 doses of the COVID-19 vaccine had been administered in The Gambia, equating to 7.5 percent of the population.
[6] Lioba A. Hirsch, “The Art of Medicine, Is it possible to decolonize global health institutions?,” The Lancet Vol. 397 (2021): 189-190.

Comments are closed