By: Michaela Clark, 2022-2023 Art Hx Interpretive Fellow
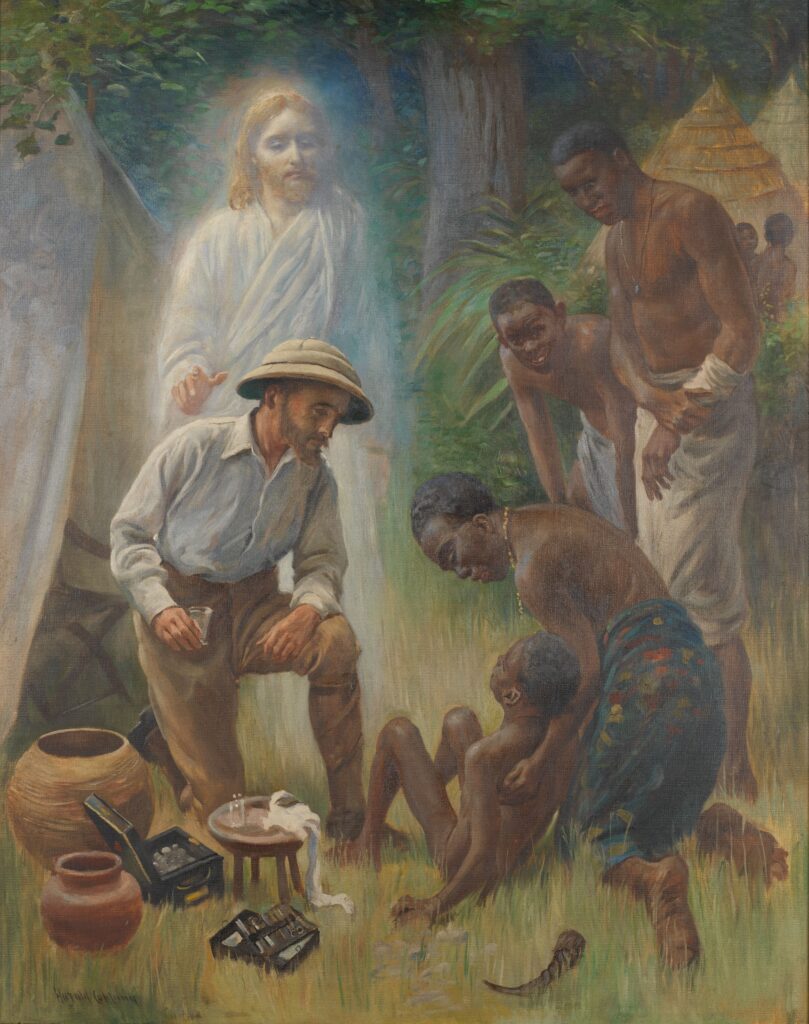
The Healer (1916) is a large oil painting made by English artist Harold Copping (1863-1932). Formerly titled A Medical Missionary Attending to a Sick African, it was commissioned by the London Missionary Society and once hung in the reading room of the Wellcome Collection—a British museum and library focused on the history of medicine, health, and healing. While it was on display for many years, it has been removed from view and placed in storage.[1] Here, it awaits a decision as to whether it should be displayed once more and, if so, how its context and content should be addressed. This is because the painting personifies multiple colonial stereotypes: it glorifies western medicine, the Christian church, and the white savior while depicting Black patients as naked (to be read as uncivilized), in awe (grateful), and ill-equipped to deal with disease (medically backward). In essence, it communicates what Europeans believed they could bring to “dark” and “sick” Africa.
These stereotypes permeate discussions about Black bodies and disease across the African continent into much of the twentieth century. An example is The Sick African (1943), a book written by South African-born physician Michael Gelfand. The title of this publication confirms the linking of Africa and its people with pathology, connecting blackness and indigeneity with illness. Within the pages of this book, Gelfand further describes his patients as ignorant or irrationally suspicious of western medicine. In addition to being noted as ineffective, indigenous healing practices are often called “uncivilized” and “barbaric” or associated with “quackery” and “sorcery.” In sum, the text and its author delegitimize local medical knowledge and indigenous healing traditions. Only medicine (as defined by Western standards) can offer freedom from disease.
In framing Western medicine as bringing salvation and health, both The Healer (1916) and The Sick African (1944) omit the fact that Western medical practices were rarely altruistic within the context of British colonialism. Much was also done to ensure white health, as settlers feared “exposure” to diseases unfamiliar to those from more temperate European climates. Indeed, public health measures frequently served as a means to disenfranchise people of color by associating them with (often contagious or stigmatizing) disease.
A case and point can be seen in South Africa, where outbreaks of bubonic plague between 1900 and 1910 legitimized the relocation of African, Indian, and mixed-raced groups in cities across the country.[2] Despite statistical evidence to the contrary, medical officials blamed people of color, arguing that certain population groups were causing the spread of this disease. Ultimately, these “risky” communities were moved to designated areas outside of the prosperous city center—demonstrating how contagious conditions could be used to justify racial segregation.[3]
Similarly, venereal disease, especially syphilis, could foster public health panic along lines of race as well as gender and class. In Europe and North America, this disease had long been associated with immorality and promiscuity; and, by the nineteenth century, scientific discussions intimately connected this disease to “abnormal” sex organs and the black female body.[4] In mid-twentieth century South Africa, this conflation played out in material ways. Here, many domestic workers were women of color who travelled from distant, often rural parts of the country to work in white homes in urban centers. The threat of racial intermixing presented by this sharing of domestic space was compounded by a fear of disease.[5] Syphilis was key to a public health panic in the 1930s and 1940s that saw invasive investigations, criminalization, and prejudicial travel and work restrictions applied to these women. While state action was framed as offering care—for individuals and society at large—it also harmed those already vulnerable to disenfranchisement. On top of stigmatizing associations and contagion fears, legislation severely compromised quality of life, harming those linked by race, class, gender, and labor.
White health was not the only concern for state officials in South Africa. During the late nineteenth and early twentieth centuries, yaws emerged as a racialized threat to this country’s labor supply. In South Africa, it was often called “native syphilis” and seen as a threat to the health (and thus the productivity) of black laborers in the mining industry.[6] Although it could affect all bodies, the disease was widely aligned with tropical climates and race-based susceptibility. Across the globe, this bacterial condition was frequently associated with syphilis, and medical discussions often merged yaws with ideas of dirt, disfigurement, promiscuity, and poverty as well as being Black. Indeed, North America and the Caribbean fostered similar notions around yaws in the 18th and 19th century, highlighting the transnational and intercontinental dimension of colonial medical ideas. In this latter context, yaws was frequently referred to as an “African disease” and a “slave malady”.[7] As in South Africa, it was deemed to be devastating to the overall health of those infected—in this case, the enslaved plantation worker.
In an effort to curb this disease in his Black, laboring patients, John Thomson (a Scottish missionary and plantation doctor in Jamaica) sought to identify, describe, treat, and cure yaws. One outcome of his research is a medical illustration titled “Stages of the Eruption in Yaws” (1819). At first it looks rather innocuous—a neutral, close-up depiction of skin lesions. But, as art historian (and Art Hx Project Lead) Anna Arabindan-Kesson has uncovered, the drawing is a direct result of observing yaws progress in a three-year-old black child whom Thomson intentionally infected.[8] This act was an attempt to achieve what had been done with smallpox inoculation: by purposely infecting a subject with a milder, non-deadly, yet related disease, Thomson hoped to abate severe symptoms and even death.
In Thomson’s mind, he was testing a method that might prove to prevent future harm. However, the doctor’s actions also resulted in the intentional infection of a child with an incurable disease. Beyond this individual harm, Thomson’s experimentation and clinical observation were also built into a larger colonial ecosystem that sought to ensure the extraction of natural resources and the maximization of financial gains. By studying it, work like that of Thomson not only perpetuated an alignment of blackness and pathology but also operated to secure financial gains of empire by curing a disease that threatened the productivity and profitability of plantations.
But medical investigations of this kind could have additional, if somewhat paradoxical, consequences. At the same time that Black bodies were seen as inherently different in relation to Western medicine’s white norms, people of color could be nonetheless abstracted and used as general examples for research and education.[9] In the context of North America, this is clearly illustrated by the now notorious obstetric experiments of James Marion Sims. Like Thomson’s inoculation of children, Sims’s investigations were conducted on the already disenfranchised—notably Black enslaved and Irish working-class women. The scientific knowledge gained from these bodies was frequently applied to benefit a white elite by keeping Black women fertile for (and thus valuable to) plantation owners.[10] However, the outcomes of Sim’s investigations on people of color were also deemed universally applicable. This was not deemed to racialized knowledge limited to the population groups experimented on. Instead, the techniques developed by Sims were used to treat white middle-class patients despite popular and scientific understandings of inherent difference between races, especially as this related to reproductive health.
On the one hand, race could be treated as a biological, bodily quality, with members of different racial groups read to have unique anatomical traits and to suffer from distinct diseases. At the same time, the bodies could also be abstracted and taken as general exemplars and the results of experiments applied across racial lines. The consequence is that Sims could use the knowledge gained from enslaved bodies on a privileged patient group, allowing him to obtain not only surgical expertise but also professional prestige. While the enslaved or immigrant status of the women was fundamental to Sims’ access to bodies for experimentation, their racial identities and ethnic otherness were ultimately “white-washed.”[11]
South Africa could similarly see race recede as a clinical concern when it served the professional interests of medical men. A case in point is the publication record of a man known as South Africa’s “Father of Surgery,” Charles Frederick Morris Saint. Born, raised, and trained in Britain, Saint made a name for himself in mid-20th century Cape Town, where he worked as the first surgical chair at the country’s first medical school. During his tenure, Saint commissioned hundreds of photographs of patients drawn from a racially diverse population. Surprisingly, the photographs commissioned by Saint appear unusual as they lack overt colonial coding. Produced in Cape Town’s urban teaching hospitals, they largely elide the kind of “tropical” or “exotic” atmosphere that historians like Nancy Stepan identify in much colonial medical imagery.[12] Instead, the photographs reveal universalizing aspirations.
This visual discrepancy is clear in Saint’s use of these South African photographs in international publications such as his book An Introduction to Surgery (1935). The text was co-authored by Saint and his mentor, James Rutherford Morison—a celebrated surgeon in Newcastle-on-Tyne, England. It was added to international libraries and reviewed by medical journals across the globe that promoted it as a general guide, useful to all surgical students. The book contains photographs of patients spanning racial groups, all used to showcase “basic principles” and the outward signs of common surgical conditions. In order to focus attention on symptoms, patients are generally stripped of contextualizing markers: they are frequently naked, the backgrounds are often erased. Not only does this communicate a neutral scientific “look,” but the time, place, and conditions of their making remain largely invisible to the viewer.
This can be seen in the coupling of three images used to demonstrate the inexplicable yet conspicuous swelling of the abdomen. Arranged as a trio or triptych, two clinical photographs (images of patients) show a young male child, undressed, and standing in profile (viewed from the side) to highlight his distended middle. These photographs flank a detailed illustration of two organs. These are colons—one is small and healthy and the other hugely enlarged. Seeing the patients and the specimens together allows the reader of the book to identify internal changes in the body—from a healthy large intestine to a diseased one (the pathological features)—with respect to what would be seen on the outside (the clinical features). All three images appear timeless and removed from any identifiable place. Without any visual markers to anchor context, they operate as universal exemplars.
However, there are conspicuous visual as well as contextual differences between the photographs. Despite their apparent neutrality, the children imaged would have then, as well as now, been categorized differently in terms of race. The photograph on the right (Fig. 169) was sourced from England prior to 1910. Standing on an ambiguous black surface before a dark grey background, the child appears very pale. His skin is almost translucent, the same shade of white as the paper on which his image is printed. In comparison, this contrast is inverted in the photograph on the left (Fig. 167). Here, the entire background (both wall and floor) is a pale gray and has been clearly erased and flattened through darkroom processing. The child’s body and hair appear dark against it. While undated and unattributed, the original record (currently in an archive at the University of Cape Town) reveals that he was photographed while standing in a large cot, situated in one of South Africa’s public hospitals around 1934.
The accompanying captions in the book do not remark on this contextual difference between the photographs. Neither the time between their making (over 20 years) nor the geographic distance (over 13 000 km / 8000 miles) are noted. There is also no mention of race in either the publication or the archival sources. This is unusual because, not only were medical texts frequently relating race to disease occurrence across the globe, but 1930s South Africa bore witness to ever increasing segregationist initiatives. When this text was published, South African society was divided into not just two race groups (White and Black) but into multiple categories, setting up highly ambiguous divisions between individuals deemed to be of European, Asiatic, African, or Indigenous and mixed descent.
Yet, the textbook written and illustrated by Saint, South Africa’s “Father of Surgery” denies this context. Posed as fundamental, core, and (ultimately) universal knowledge, it avoids the settler-colonial and segregationist setting in which much of its contents were produced. This allows the patients depicted to emerge as exemplary “teaching material” no matter the color of their skin. Indeed, as black and white images, race remains uncertain throughout. The shifting tone and inconsistent contrast makes projecting South Africa’s race-based divisions difficult. The result is that race is a conspicuous but unstable feature. It is both ever-present and invisible, functioning as an elusive signifier that highlights the slippery nature of racial categories and medicine’s attitudes towards them.
Looking beyond national borders and across visual media allows for the tension between clinical care and imperial harm as well as the ambiguous place of race in medicine to be glimpsed. The painting, illustrations, photographs, and publications discussed here demonstrate how the conflict within care/harm and the presence/absence of race work at the heart of colonial medicine. First, western medical activities suggest concern for people of color. But in practice clinical work was often extractive and exploitative, preventing or curing disease to ensure a productive labor force, assuage white fears, or to use as experimental or teaching material. Western medicine was a double-edged sword: while many doctors (particularly British missionaries) believed it would “save” local people from ill health, frequently the corollary to care was colonization and conquest. Second, to function within the colonial context, medical ideas were forced to constantly negotiate questions around racial difference. Sometimes race was key to making sense of disease, while in other instances it was willfully ignored. Ultimately, race mattered, and many careers were built off differentiating humans and disease along racial lines. But it could also recede when acknowledging it hindered medical and professional progress.
Footnotes
[1] Wellcome Collection Library Catalogue, “The Healer,” Accessed January 5, 2023, https://wellcomecollection.org/works/u4hc2hwe.
[2] Howard Phillips, “Plague, 1901-1907: ‘The dreaded disorder,’” in Plague, Pox and Pandemics (Johannesburg: Jacana, 2012): 38-67.
[3] Maynard Swanson, “The Sanitation Syndrome: Bubonic Plague and Urban Native Policy in the Cape Colony, 1900-1909,” The Journal of African History Vol. 18, no. 3 (1977): 387-410.
[4] Sander Gilman, Difference and Pathology: Stereotypes of Sexuality, Race, and Madness (Ithaca and London: Cornell University Press, 1985).
[5] Karen Jochelson, The Colour of Disease: Syphilis and Racism in South Africa, 1880-1950 (New York: Palgrave, 2001).
[6] Jochelson, The Colour of Disease. Megan Vaughan, Curing Their Ills: Colonial Power and African Illness (Cambridge & Malden: Polity Press, 1991).
[7] Londa Schiebinger, Secret Cures of Slaves: People, Plants, and Medicine in the Eighteenth-Century Atlantic World (Stanford: Stanford University Press, 2017). Similar attitudes to Yaws can be seen in South Africa, with the disease frequently called as “native syphilis” in the early twentieth century. See Jochelson, The Colour of Disease.
[8] Anna Arabindan-Kesson, “Transmission and Transfer: Plantation Imagery and Medical Management in the British Empire,” Art History Vol. 45, no. 3 (2022): 448-703.
[9] Christopher DW Willoughby, Masters of Health: Racial Science and Slavery in U.S. Medical Schools (Chapel Hill: University of North Carolina Press, 2022).
[10] Deirdre Cooper Owens, Medical Bondage: Race, Gender, and the Origins of American Gynecology (Athens: The University of Georgia Press, 2017).
[11] Owens, Medical Bondage, 112.
[12] Nancy Leys Stepan, Picturing Tropical Nature (London: Reaktion Books, 2001).

Comments are closed